Quick guide 2026 (no confusion)
If you want the cost of a complete implant (implant + abutment + crown + surgery and follow-ups), visit our main guide:
Dental implant cost in Colombia 2026 (Complete guide)
.
For patients in the United States planning treatment in Colombia
- Remote pre-check (optional): You can send photos and any recent scans (if you have them) so we can guide you on likely options before you travel.
- Travel planning: Many international patients schedule a short trip for evaluation and the first clinical phase, then follow the recommended check-ups before returning home.
- Clear written quote: After evaluation, we provide an itemized plan so you can compare “per-unit” vs “complete implant” costs and avoid surprises.
Schedule an evaluation: Contact us. If you prefer, you can also review our main guide above for the full “complete implant” cost explanation.
When someone asks “how much does a dental implant cost?”, two different things often get mixed up:
- Per-unit cost: the implant component (the “screw”).
- Complete implant cost: implant + abutment + crown + surgery + follow-ups.
There’s also a key point to avoid confusion: at our clinic we work with two implant approaches with different
timelines and costs:
- Conventional implantology (traditional staged protocol).
- Strategic immediate-load implantology (corticobasal / compressive—case-dependent), which may allow fixed provisional teeth in 24–48 hours in selected cases.
1) Key difference: “per unit” vs “complete implant”
Per unit usually refers only to the implant itself (the screw). Many offers are advertised this way, and later the patient discovers that key parts or services are missing.
In practice, most patients end up paying for the complete implant, which typically includes:
- Implant
- Abutment (connector)
- Crown (the visible “tooth”)
- Surgery + follow-up visits
👉 To understand the real total cost, see:
Complete dental implant cost in Colombia 2026
.
2) 2026 quick table: per-unit implant, crowns & common add-ons
Indicative ranges may vary by diagnosis, complexity, and materials. Final pricing is confirmed after a clinical evaluation.
| Item | Indicative range (COP / USD*) | What it means |
|---|---|---|
| Implant per unit (screw) | COP $1,900,000 – $2,300,000 (≈ USD $495 – $600*) | Typically does NOT include abutment, crown, or full surgery/follow-ups. |
| Abutment | (depends on system & case) | Connector between the implant and the crown. Sometimes included in full plans. |
| Porcelain-fused-to-metal crown (PFM) | COP $1,800,000 – $1,900,000 (≈ USD $470 – $495*) | Functional and often more economical (case-dependent). |
| Zirconia crown | COP $2,000,000 – $2,200,000 (≈ USD $520 – $570*) | High aesthetics and strong performance in many cases. |
| Simple extraction (if needed) | COP $150,000 – $350,000 (≈ USD $40 – $90*) | When a tooth must be removed before the implant. |
| Bone graft / guided bone regeneration (if needed) | COP $800,000 – $5,000,000 (≈ USD $210 – $1,300*) | Depends on type and volume. Learn more: bone regeneration. |
| Sinus lift (if needed) | COP $3,000,000 – $5,000,000 (≈ USD $780 – $1,300*) | Upper jaw procedure to gain bone height in selected cases. |
| Conscious sedation (if needed) | (depends on duration/procedure) | Helpful for anxiety or longer treatments. See: conscious sedation. |
Tip: if an “offer” only mentions the implant screw price, always request a written breakdown including:
implant + abutment + crown + surgery + follow-ups.
3) Scenario “calculator”: how to estimate your case
Think of total cost as a sum of “blocks”. The base block is often implant + crown,
and then (depending on diagnosis) you may add extraction, bone grafting/regeneration, sinus lift, sedation, etc.
Scenario A: simple case (no graft) + crown
- Implant per unit (reference): COP $1,900,000 – $2,300,000 (≈ USD $495 – $600*)
- Crown (PFM or zirconia): COP $1,800,000 – $2,200,000 (≈ USD $470 – $570*)
- Key point: the real total is usually higher because it may not include abutment/surgery/follow-ups. For the real total, see the main guide (complete implant).
Scenario B: with extraction beforehand
- Extraction: COP $150,000 – $350,000 (≈ USD $40 – $90*)
- Then add the implant + crown plan (based on diagnosis)
Scenario C: bone loss (requires regeneration/grafting)
If bone height/width is insufficient, a conventional implant may require grafting or guided bone regeneration.
Learn more here: Bone regeneration.
- Graft/regeneration: COP $800,000 – $5,000,000 (≈ USD $210 – $1,300*)
- Then the implant + crown plan
- Impact: it may increase treatment time and budget (the type of graft influences outcomes and follow-ups). [R2]
Scenario D: alternative to optimize time (selected cases)
In selected cases, strategic implantology (cortical anchorage / compressive implants and immediate-load protocols)
may help avoid grafting in many cases and/or reduce clinical time.
See:
Strategic implantology
and patient experience:
strategic implants in 24 hours.
| Scenario | What changes the budget | What to ask for in the quote |
|---|---|---|
| Simple | Crown material, abutment type, number of follow-ups | Implant brand/system, abutment included or not, crown type, follow-up plan |
| With extraction | Extraction complexity and site management | Whether extraction, meds, and post-op control are included |
| With graft/regeneration | Bone volume, biomaterials, clinical time | Type of graft, membrane (if used), healing time, follow-ups |
| Sinus lift | Technique, biomaterial, anatomy complexity | Whether sinus lift, follow-ups, timeline, and meds are included |
| Sedation | Procedure duration and clinical need | Scope of sedation/monitoring per protocol and what it covers |
4) Strategic implantology (immediate load / corticobasal): what it is and when it’s considered
In addition to conventional implantology, our clinic works with strategic immediate-load implantology,
also known as corticobasal (and/or protocols using compressive implants depending on the case).
⚠️ Important: this approach is not used only when there is “no bone”.
In many cases it’s considered as an alternative to:
- Avoid grafting in many cases (when diagnosis allows).
- Reduce clinical timelines.
- Deliver fixed provisional crowns within 24–48 hours.
- Implants may anchor in cortical bone (more stable) or in alveolar bone using compressive implants.
- Choosing basal vs compressive implants depends on the diagnosis and available bone.
- The goal is to achieve stability for immediate loading when clinically indicated. [R4]
👉 Full guide:
Strategic implantology
5) 2026 costs – Strategic implantology (immediate load)
🔹 Front teeth & premolars
(incisors, canines, premolars)
- Total cost per tooth: COP $4,900,000 (≈ USD $1,275*)
- Phase 1 (24–48 hours): COP $3,100,000 (≈ USD $805*) — implant + fixed PMMA provisional crown
- Phase 2 (within 8 to 18 months max): COP $1,800,000 (≈ USD $470*) — upgrade to definitive zirconia crown
🔹 Molars (high-load zones)
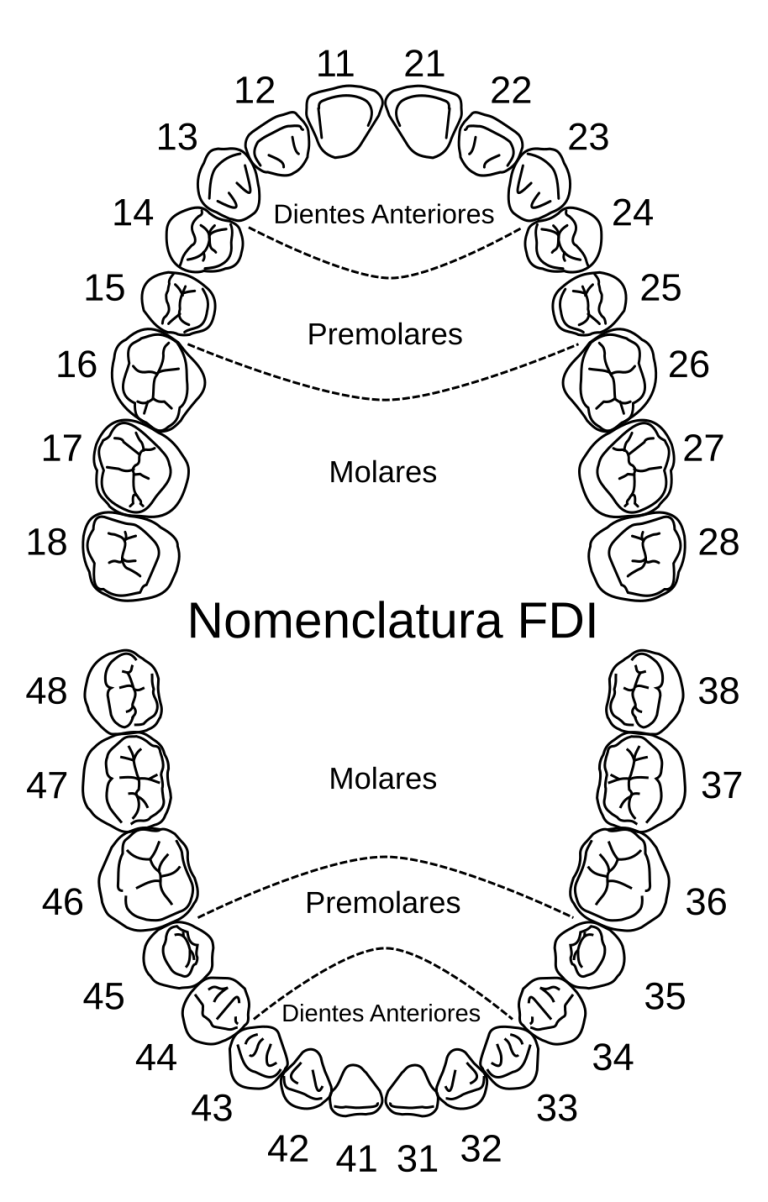
(first and second molars: 16, 17, 26, 27, 36, 37, 46, 47)
For molars, due to chewing load, it’s common to require 2 implants to support 1 crown (when it’s a single isolated molar).
- Total cost per molar: COP $5,900,000 (≈ USD $1,535*)
- Phase 1 (24–48 hours): COP $4,100,000 (≈ USD $1,065*) — 2 implants + fixed PMMA provisional crown
- Phase 2 (within 8 to 18 months max): COP $1,800,000 (≈ USD $470*) — upgrade to definitive zirconia crown
Clinical note: when two consecutive molars are needed (e.g., 36 and 37), in some cases 3 implants may be placed to support 2 crowns.
Tooth numbering (visual clarification)
To avoid confusion, “molars” here refer to: 16, 17, 26, 27, 36, 37, 46, 47.
6) Conventional vs strategic: quick comparison
| Aspect | Conventional | Strategic (immediate load) |
|---|---|---|
| Timeline | Months until the definitive crown | 24–48 hours for a fixed provisional crown (when indicated) [R4] |
| Grafting | More frequent in some cases | Often avoided in many cases (diagnosis-dependent) |
| Anchorage | Alveolar bone | Cortical or compressive anchorage (case-dependent) |
Key phrase (to avoid confusion):
The cost of an implant depends on whether it’s done using conventional implantology or
strategic immediate-load implantology. These are different protocols with different timelines, indications, and budgets.
7) PFM vs zirconia: which crown is better?
The crown is the visible part that “looks like a tooth”. Choosing a material isn’t only about aesthetics—it can also affect strength, fit, and maintenance.
PFM (porcelain-fused-to-metal)
- Can be a functional and more economical option.
- Often used in posterior areas (depending on aesthetics needed).
Zirconia
- Excellent aesthetics in many patients.
- High strength and widely used in modern rehabilitations.
- There are reviews comparing materials for implant-supported prostheses. [R5]
Key point: it’s not just “which material is best”, but which one fits your bite, gums, and the tooth area.
If you have bruxism (clenching/grinding), the plan and maintenance become even more important.
8) Related scientific evidence (specific readings)
Below are specific readings related to topics covered in this article:
peri-implant risk, bone regeneration, sinus lift, immediate/early loading, and prosthetic materials.
- Peri-implant risk and periodontal history: history of periodontitis is associated with increased risk of peri-implantitis.
PubMed: 30391683 - Guided bone regeneration (GBR): systematic review including outcomes and factors such as membrane exposure.
PubMed: 29368353 - Sinus lift: meta-analysis on implant survival associated with sinus augmentation procedures.
PubMed: 36511050 - Immediate/early loading: systematic review comparing outcomes (depending on stability criteria and case selection).
PubMed: 29703670 - Zirconia vs metal-ceramic in implant-supported rehabilitation: systematic review in implant-supported prostheses.
PubMed: 38425320
Note: These references are for learning the clinical “why”. Final indication always depends on your individual diagnosis.
9) Step-by-step: what you usually pay for (and why)
One reason quotes differ so much is that not all plans include the same items.
This step-by-step helps you spot what may be missing.
1) Diagnosis
- Clinical exam, gum evaluation, and bite analysis.
- Define whether extraction, regeneration, or complementary procedures are needed.
2) Implant surgery
- Implant placement and post-op follow-up.
- In some cases: soft tissue management, sutures, and extra visits.
3) Abutment + records
- The abutment connects the implant to the crown (it’s not always included when the quote is “per unit”).
- Records and try-ins depending on the prosthetic plan.
4) Final crown + bite adjustment
- Delivery of the crown (material depends on the case).
- Bite adjustments to reduce overload.
5) Follow-ups and maintenance
- Check-ups to monitor gums, hygiene, inflammation, and stability.
- Maintenance plan depends on risk (hygiene, smoking, diabetes, bruxism, periodontal history). [R1]
10) Checklist: what a serious implant quote should include
Before deciding, request a written quote that answers:
- What is the implant brand and system?
- Is the abutment included or quoted separately?
- Which crown type is included (PFM vs zirconia) and when does it change?
- Does it include surgery, post-op follow-ups, and how many follow-up visits?
- What happens if extraction, grafting, or sinus lift is needed (included or “quoted later”)?
- Are bite adjustments included, and what’s recommended if you have bruxism?
- What are the warranty conditions and the maintenance plan?
11) Maintenance: what protects your investment (and almost nobody explains)
An implant doesn’t “take care of itself”. Long-term stability depends on healthy gums, hygiene, follow-ups, and risk-factor control.
That’s why an overly “cheap” quote can become expensive if it doesn’t include education, follow-ups, and maintenance. [R1]
Early warning signs
- Bleeding when brushing or using floss/interdental brushes.
- Persistent bad odor.
- Swelling or redness around the implant.
- Pain or discomfort when biting (not always normal).
Practical recommendation
- Schedule periodic follow-ups (frequency depends on your risk profile).
- Use the right interdental tools (we prescribe them based on your case).
- If you have bruxism, consider an occlusal guard (when indicated).
Want a real quote for your case?
Final cost depends on diagnosis (bone, gums, bite, area) and on the indicated approach (conventional vs strategic).
If you want, we can guide you with an evaluation.
Related articles
Does this article show the total cost of a complete implant?
No. This page shows the per-unit implant breakdown, crowns, and scenarios that change the budget, plus a comparison between conventional and strategic approaches. For the total cost of a complete implant, see the main guide linked at the top.
What does “per-unit cost” mean for a dental implant?
It usually refers to the implant component (the “screw”) and may not include the abutment, crown, surgery, follow-ups, or additional procedures.
Why can the per-unit implant (screw) range vary by city or case?
It can vary due to availability, logistics, implant system, and case complexity. These are indicative 2026 ranges; final pricing is confirmed after evaluation.
How much does an implant crown cost?
It depends on the material and the lab. PFM crowns are often more economical, while zirconia tends to offer higher aesthetics and strong performance in many cases.
What usually increases implant cost the most?
Additional procedures (grafting/regeneration, sinus lift, extractions), crown material, and overall case complexity.
When is bone grafting or regeneration needed?
When there isn’t enough bone volume for predictable stability with conventional implantology. This is confirmed through evaluation and imaging.
Is strategic implantology only for people with severe bone loss?
No. In selected cases, it can be considered to avoid grafting in many cases and/or reduce timelines and deliver fixed provisional crowns within 24–48 hours, when the diagnosis allows.
How can I tell if a quote is incomplete?
If it only mentions the implant “screw” price and doesn’t specify abutment, crown type, surgery, follow-ups, implant brand/system, and warranty/maintenance conditions.
What should I ask before choosing where to get an implant?
A complete diagnosis, a written itemized quote, the implant system/brand, a follow-up/maintenance plan, and clear warranty conditions.

Author
Dr. Johanna Calderón
Periodontics & implants specialist. Our clinic has a team of specialists providing comprehensive care:
dental implants, periodontics, smile design, endodontics, and general dentistry.
We treat national and international patients and guide you with a clear plan based on your diagnosis
(bone, gums, bite, and the area to rehabilitate).
Last updated: 01/01/2026.